Retained Hemothorax: An Unusual Case
/Background on hemothorax and its management
Traumatic hemothorax occurs frequently, with up to 300,000 cases occurring yearly in the United States.1 In cases of polytrauma, head and chest injuries frequently occur together,2 and thus it is important for all neurointensivists who see TBI to understand management of common traumatic chest injuries, including hemothorax. While some small hemothoraces (<300cc’s) can be monitored clinically, standard of care for most large traumatic hemothoraces is rapid tube thoracostomy.
So, why do we do tube thoracostomy and not a less invasive procedure, like thoracentesis, for patients that look well? Well, we have an unusual case from which to learn.
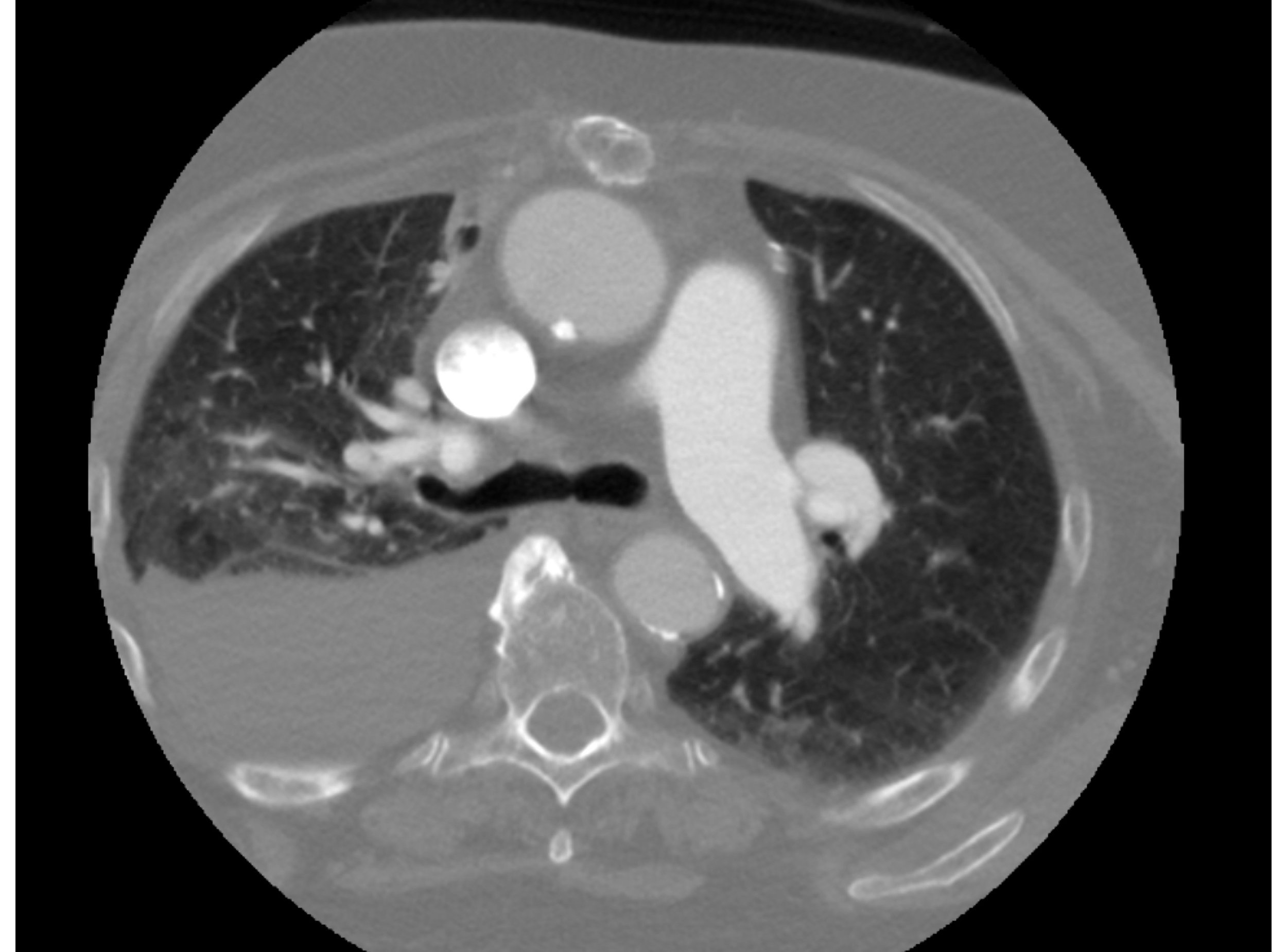
Figure 1: CT-angiogram of neck identifies significant pleural fluid collection
Case History
An 83-year-old woman with a history of atrial fibrillation (not on anticoagulation due to falls) presented with a R MCA stroke. She was not given IV tPA, as her family reported a history of hemothorax after a fall 1.5 weeks prior to onset. Instead, she was taken for thrombectomy with TICI 2B reperfusion; he symptoms improved modestly after the procedure. She was then brought to the neuroscience ICU.
She was noted to be slightly tachypneic, although an ABG showed excellent oxygenation and ventilation (7.29/32/142 on 2L NC). The team reviewed her CT-angiogram of the neck to see if there was any lung pathology, which is shown in Figure 1.
The CT showed a moderate-large size R pleural fluid collection. We reviewed records from her recent hospitalization. She had presented dyspneic and was found to have a R pleural fluid collection; she underwent a thoracentesis with 1.5L of blood drained. When they found the blood, they took more history and found that she had fallen lately and confirmed multiple R-sided traumatic rib fractures. Since they had obtained a lot of fluid and she looked well, the decision was made to observe her clinically. She was discharged home clinically stable and developed her RMCA stroke while at home. Our CT revealed incidentally that she was suffering from a retained hemothorax.
What is a retained hemothorax and why is it a problem?
A retained hemothorax is typically defined as >500cc’s of persistent blood after initial drainage of a hemothorax, or any significant amount of blood unsuccessfully drained after 72 hours of thoracostomy.4 Many patients with retained hemothorax do not present with ventilation or oxygenation problems, meaning that you have to be vigilant about looking for it. If a retained hemothorax is not treated adequately, the biggest concern is that the patient will develop an empyema, which happens with nearly 30% of retained hemothoraces.5
So, even in a well-appearing patient, a large persistent traumatic hemothorax needs to be drained in most cases, and NOT with thoracentesis, which just cannot clear enough blood out. If you find yourself in the rare circumstance that you do a thoracentesis and stumble onto a traumatic hemothorax, assume the patient will need more drainage regardless of how much blood you get. Options are a tube thoracostomy, suction assisted tube thoracostomy, or a video assisted thorascopic surgical (VATS) procedure. Call your local trauma surgeon early.
Back to the case
In our case, we called the trauma service, and they performed a suction assisted tube thoracostomy at the bedside, with drainage of ~800cc’s of blood. The patient had a chest tube in place for about 72 hours and then did well, with no residual hemothorax. Her tachypnea resolved, and she was discharged from the hospital to rehab after 10 days.
REFERENCES
Richardson JD, Miller FB, Carrillo EH, Spain DA. Complex thoracic injuries. The Surgical clinics of North America 1996;76:725-48.
Huang FD, Yeh WB, Chen SS, et al. Early Management of Retained Hemothorax in Blunt Head and Chest Trauma. World journal of surgery 2018;42:2061-6.
Demetri L, Martinez Aguilar MM, Bohnen JD, et al. Is observation for traumatic hemothorax safe? The journal of trauma and acute care surgery 2018;84:454-8.
Smith JW, Franklin GA, Harbrecht BG, Richardson JD. Early VATS for blunt chest trauma: a management technique underutilized by acute care surgeons. The Journal of trauma 2011;71:102-5; discussion 5-7.
DuBose J, Inaba K, Okoye O, et al. Development of posttraumatic empyema in patients with retained hemothorax: results of a prospective, observational AAST study. The journal of trauma and acute care surgery 2012;73:752-7.